Yusra Munir
Derpartment of Pharmacy
Bahauddin Zakariya University, Multan.
Pakistan, a country over a 220 million population omitting a vibrant culture possess healthcare system that has been deteriorating steadily over the years, leading to dire consequences for the health and well-being of its inhabitants. In this mosaic of health challenges, one stands with grim statistic that is one of the highest maternal mortality ratios (MMR) in the world with the notorious percentage of 14.4% [1], as illustrated below in the pie chart, making it third leading country in South Asia in maternal mortality deaths. The question which arises is, who stands accountable for the statistics? Is it the government, the individuals, the healthcare system, or all of them.
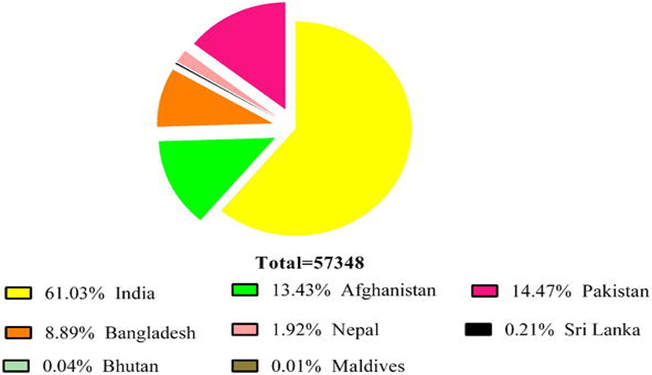
Figure 1: The number of maternal deaths in the region of South Asia. Stats by the World Health Organization on maternal mortality trends 2000–2017 estimates that South Asia accounts for 57,000 maternal deaths [1].
The statistics:
According to a survey recently conducted by National Institute of Population Studies which USAID funded “Pakistan Maternal Mortality Survey 2019’ shows marked variation in the maternal mortality rate of women living in urban and rural Pakistan areas. 186 deaths per 100,000 live births is the ratio of Pakistan’s maternal mortality [1]. In Pakistan in 2019, 186 deaths per 100,000 livebirths has also been reported, which is from 2017 about 32% increase (140/100,000 livebirths) [2].
Major issues associated with MMR:
- Lack of Education:
A significant portion of Pakistan’s population lacks adequate knowledge about maternal health, family planning, and the importance of antenatal and postnatal care. Antenatal care involves examinations, ultrasounds etc. before delivery while postnatal care involves almost 6 weeks after delivery. Among the maternal characteristics in the Pakistani site compared to the other sites, the one that stands out the most is lack of formal education. Nearly 83% of Pakistani women had no formal education compared to only 12% in the other sites combined. National reports by UNICEF and the PDHS have highlighted that low educational level is a key factor associated with poor access to critical maternal health services as well as poorer maternal and child health outcomes [3].
Here, the responsibility extends to both the government and civil society to promote comprehensive health education and awareness campaigns.
- Access to skilled healthcare providers and infrastructures:
A shortage of skilled healthcare providers, particularly in remote areas, exacerbates Pakistan’s maternal health crisis. The lack of doctors, nurses, and beds in government hospitals also contributes to the high maternal mortality rate in the country. Most regular staff members are postgraduate trainee’s incapable of dealing with pregnancy-related complications. This is presumably due to inadequate experience and exposure [4].
Especially women residing in rural areas, lack basic health facilities. A great number of pregnant women die while travelling to the hospitals which are far off in the cities. For the reason most of them give birth at home which is extremely common is remote areas. A total of 74% of women in rural areas give birth at home, compared to 43% of women in urban areas [4]. The responsibility for producing and retaining healthcare professionals, including doctors, nurses, and midwives, rests on both the government and educational institutions. Additionally, measures should be taken to incentivize healthcare professionals to work in underserved regions.
- Socio cultural factors:
Many Pakistani women specially the one living in remote areas are victims of outdates practices of customs and cultures. Child marriage is very common in rural areas with girls mostly of age 16 while boys of age 18 on an average. Surprisingly, women also get married at the age of fourteen. This issue along with, limited decision-making power for women, and cultural practices often contribute to high-risk pregnancies. Addressing these deep-rooted socio-cultural factors requires a collaborative effort from religious leaders, community influencers, and non-governmental organizations.
- Policy and governance:
Unfortunately, Pakistan lack in policy making when it comes to healthcare facilities. One of the major leading causes of poor health practices. When it comes to MMR, effective health policies like family planning programs, budget allocation, resource distribution, building healthcare infrastructures and force work, accountability mechanisms, Awareness campaigns etc. are effective in addressing the MMR.
- Indigence:
MMR is indeed closely related to poverty. Recent trends illustrate 1/4th of entire population resides below the poverty line. With the majority inhabiting in remote areas, 31% of the rural individuals impoverished in comparison to 13% urban population [5]. This major difference between these two communities omits a great risk of reproductive health related problems like their kids are more prone to undernourishment and malnutrition [1].
| Attributes | Women with no education | Provincial distribution of uneducated women | |
| Residence | Rural | Urban | |
| Level of schooling | 62.3% | 33.6% | Total uneducated = 51.7% |
| Punjab | 50.5% | 27.2% | 41.7% |
| Sindh | 82.4% | 36.5% | 57.1% |
| Khyber Pakhtunkhwa | 70.0% | 48.5% | 66.8% |
| Balochistan | 80.4% | 66.5% | 76.2% |
A comparison of ever-married women between the ages of 15 to 49 having no education in rural and urban areas of Pakistan according to Pakistan Maternal Mortality Survey 2019 [2].
Conclusion:
Maternal health not only belongs to the women herself but also the baby and entire family. The high maternal mortality ratio in Pakistan is a multifaceted problem that demands a multi-pronged approach. While the government bears a significant responsibility. Thus, policy and governance are foundational in addressing the high maternal mortality ratio in Pakistan. Effective policies, coupled with good governance practices, can create an enabling environment for improving maternal health outcomes, reducing disparities and ultimately saving the lives of mothers and newborns, but apart from that it is essential to recognize that addressing this crisis requires collaboration from various stakeholders, including civil society, healthcare professionals, educators, religious leaders, and communities. Intervention plays a significant role as per research which clearly demonstrate the reduction in maternal and child mortality (in Bangladesh by 66% and 65%. Cambodia 775% and 57%, China approximately 80% and 80%, Vietnam 70% and 60%) [1]. So, no matter it’s the rural or urban area, the change starts from within. Let’s make this world a better place by addressing these issues and educating others.
References
1. Muhammad, H., et al., Maternal Mortality in Rural Areas of Pakistan: Challenges and Prospects, in Rural Health, B. Umar, Editor. 2021, IntechOpen: Rijeka. p. Ch. 6.
2. Aziz, M.A., PAKISTAN MATERNAL MORTALITY SURVEY 2019. National Institute of Population Studies 2019: p. 81.
3. Aziz, A., et al., Why are the Pakistani maternal, fetal and newborn outcomes so poor compared to other low and middle-income countries? Reproductive Health, 2020. 17(3): p. 190.
4. Shaeen, S.K., et al., Maternal mortality in Pakistan: Challenges, efforts, and recommendations. Ann Med Surg (Lond), 2022. 81: p. 104380.
5. Farooq, S. and U. Ahmad, Economic growth and rural poverty in Pakistan: A panel dataset analysis. The European Journal of Development Research, 2020. 32(4): p. 1128-1150.

